I have two graduate degrees in nursing. I’ve worked in healthcare. Or rather, I’ve worked in sickness medicine and wellness or functional medicine. I understand the human body. And yet—I completely missed my own perimenopausal symptoms.
Let that sink in.
If someone with advanced clinical training can overlook such a huge physiological shift, what hope does the average woman have when she walks into her doctor’s office with anxiety, fatigue, insomnia, mood swings, and a period that’s all over the map?
Here’s the kicker: she might get an antidepressant, anti-anxiety pill or Ozempic. She might get a shrug. But she probably won’t get her hormones tested. And she almost certainly won’t get the words she needs to hear:
“You’re in perimenopause. Let’s talk about what that means.”

Wait… This Is Perimenopause?
Let’s rewind a little. Perimenopause is the transitional phase leading up to menopause, where our hormones—especially estrogen and progesterone—start fluctuating wildly. This shift can begin years before your final period. And for many women, that means their 30s.
Yes, you read that right. A recent study from February 2025 found that 25% of women aged 30–35 were already experiencing perimenopausal symptoms. But hardly any of them knew it. Most thought they were tired, overwhelmed, or just dealing with “normal aging.”
Spoiler: it’s not just aging. It’s a hormonal storm. And very few people are talking about it.
Why Doctors Don’t Catch It
This brings us to the heart of the issue—and the question that inspired the title of this blog: Is this medical gaslighting… or just ignorance?
Honestly? It’s probably a little of both.
1. Medical training doesn’t cover it
In 2020, only about 20% of OB-GYN residency programs in the U.S. reported having a formal menopause curriculum. Less than 7% of residents said they felt prepared to manage menopause-related care. And that’s menopause—we’re not even talking about perimenopause, which is even less discussed.
So, when a woman in her 30s or 40s walks in describing fatigue, anxiety, heavy periods, or insomnia, her provider often doesn’t even think to look at hormones. They’re more likely to write a prescription for an SSRI or tell her to try yoga. Case in point – when I was at my book signing event, a woman on the front row actually said that when she complained to her doctor about loss of libido, he actually said “get a new boyfriend”!
Are you kidding me? This is not only bad advice, but it’s totally ignorant, in my humble opinion. And it doesn’t help women understand the big-picture changes happening in their bodies.

2. The system doesn’t prioritize prevention
Western medicine is largely built on a “treat-the-disease” model. If you’re not infertile, pregnant, or in menopause, your hormones are often considered irrelevant. And because perimenopause is dynamic—your hormones fluctuate daily—some doctors argue that testing isn’t useful.
But here’s the thing: trends over time and symptom tracking absolutely can tell a story. And women deserve doctors who are willing to listen and connect the dots.
Additionally, it’s critical that women understand how their bodies metabolize estrogen—and the balance between progesterone and estrogen, often referred to as the P:E ratio. Imbalances here have been linked to an increased risk of hormone-related cancers. That’s why I often recommend the DUTCH hormone test.
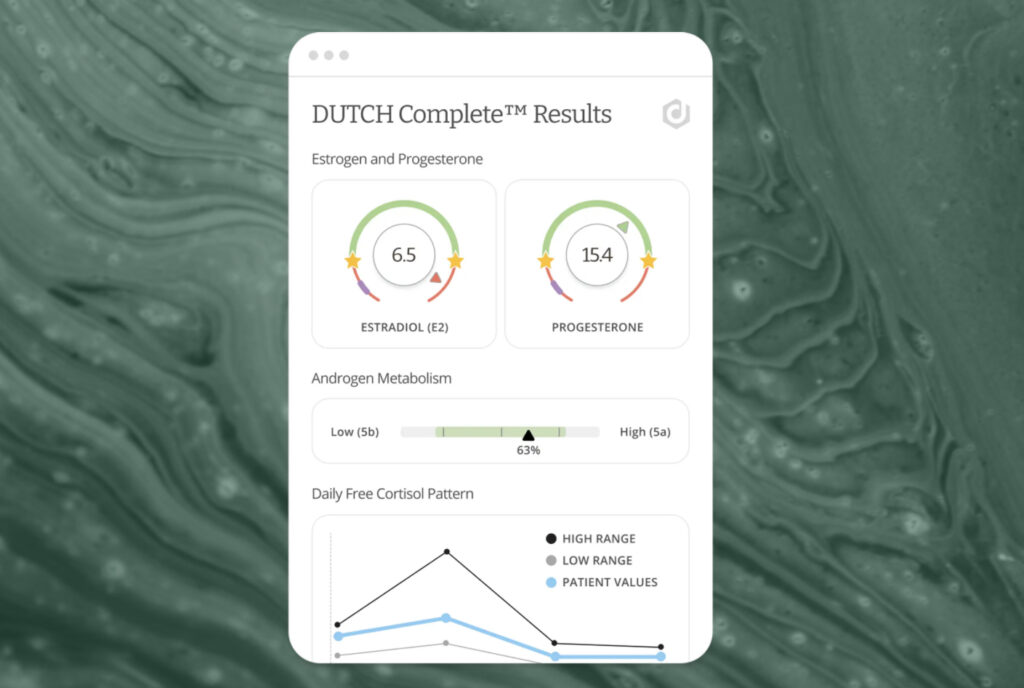
It offers a comprehensive look at hormone levels, hormone metabolism, adrenal health, and even organic acids like B vitamins, glutathione, inflammatory markers, and gut health indicators. These insights not only help uncover the root cause of symptoms but can also guide disease prevention down the road.
As Tara Scott, M.D.—an OB-GYN and international educator—says, this test “should be standard of care,” and I couldn’t agree more.
So, What Is Normal?
Here’s the twist: we’ve normalized suffering.
We expect midlife women to feel run-down, irritable, and emotionally unsteady. We blame stress. Or kids. Or caffeine. And because no one ever explained what perimenopause looks like, we just assume this is what it feels like to “age in a female body.”
This is where the cultural silence becomes dangerous. We don’t learn about perimenopause in school. A 2022 study found that over 90% of women had never been taught about menopause in school, and more than 60% said they didn’t feel informed about it at all
I’ve had friends tell me, “I thought I was losing my mind.” Others said they felt like their bodies betrayed them.
And again, just last week at my book signing event, another woman shared—almost proudly—“I haven’t had a period in nine months and I haven’t had any symptoms.” But as we kept talking, it became clear that she’d recently started having migraines and her libido had completely vanished. She was genuinely surprised to learn that both are common signs of hormonal imbalance and perimenopause.
The problem isn’t that women are out of touch with their bodies—it’s that no one has ever taught us what to look for. Once we connect the dots, the confusion fades and we can finally start to care for ourselves in a way that’s rooted in understanding, not frustration

The Gender Gap in Health
Let’s not pretend this is an isolated issue. Women’s health is underfunded, under-researched, and too often dismissed.
Until 1993, the NIH didn’t even require women to be included in clinical trials. Today, disparities still persist. One study out of Yale found that women’s reports of pain are often taken less seriously than men’s, leading to lower rates of appropriate treatment in emergency care settings
Another large-scale review revealed that women with abdominal pain were up to 25% less likely than men to receive opioid pain medications in ERs.
So when women show up with perimenopausal symptoms, it’s no wonder they’re often brushed off. We are taught to tolerate discomfort. And our providers are trained—consciously or not—to deprioritize it.
That has to change.
What Can We Do About It?
If this all sounds a bit depressing, stay with me—because there’s good news. We have *power* here. And it starts with awareness.
1. Track your symptoms
Notice how you feel across your cycle. Write it down. Patterns will start to emerge—and that data is gold when you talk to your provider.
2. Ask for the labs
Even if hormone levels fluctuate, things like FSH, estradiol, and progesterone can still provide useful context—especially when paired with your symptom history. You deserve a doctor who doesn’t dismiss that. As I’ve mentioned above, there is no better test to get the real, full picture of your hormone balance and hormone health, than the DUTCH test. While our sickness insurance (that’s what I call health insurance) still does not cover the test, HSA cards do. And, I promise it will be one of the best investments in your health and hormone balance!
3. Find the right provider
Not all doctors are created equal. Look for someone who understands perimenopause or is certified by organizations like The North American Menopause Society (NAMS). Then again as I’ve mentioned in earlier blogs, many NAMS certified docs do not understand functional medicine. I would choose Functional and integrative practitioners. I would suggest starting with DUTCH provider such as myself, to help you sort out what’s going on.
4. Talk about it
With your friends. Your sisters. Your coworkers. The more we speak openly, the more we de-stigmatize this phase of life. Perimenopause should not be a secret women discover after they’ve suffered through it.

You’re Not Crazy—You’re Changing
If you take one thing from this post, let it be this: you are not broken, weak, or overreacting. If you feel like something’s off, you’re probably right. Trust your instincts.
Perimenopause is real. It can start early. And it deserves more than a passing mention in a textbook—or a prescription without a conversation.
The problem isn’t that you’re out of touch with your body—it’s that no one ever taught you what to look for. Once you start connecting the dots, the confusion begins to lift, and you can finally care for yourself with clarity, confidence, and compassion.
If you support in connecting the dots, that’s my passion and gift. You can reach out to ConsultLori.com for a free 15 minute call.

