Breast cancer is a formidable adversary, affecting millions of women worldwide. The staggering numbers of 1:8 is climbing, expected to rise by 57% in the next 20 years, and impacting more and more young women.
Are you concerned about getting that 4-word call “You have breast cancer”?

Are you confused about what is the best screening option for you?? You’re not alone.
If you have been following me for long, you know that my focus is on prevention! Yet, early detection is important and is crucial for successful treatment and improved outcomes. Now, if you’re one of the like-minded women in my tribe, I know that you’re looking for better options than just a mammogram that smashes and radiates your breast. In this two-part blog series, I’m going to discuss various detection methods – some are very early and designed to ensure breast health (and thus why I use them in my functional medicine coaching with clients), and some are very late and dangerous.
Today, I’ll share 6 different screening methods: breast self-exams (BSE), mammography, ultrasound, MRI (Magnetic Resonance Imaging), Thermography, and the new QT imaging. We’ll discuss the differences between them, their effectiveness, and their potential benefits in the detection of breast cancer.
NOTE: next week, I will discuss screening methods to ensure breast health. I’ll share the cutting-edge, early modalities that I use personally, and incorporate into my practice.
Breast Self-Exam
I remember the early days, many decades ago in my nursing career when we started teaching Breast Self-Exams (BSE). It’s true that most lumps are found by women (or perhaps the men in their lives), so this method is helpful. Yet even this is not an “early” detection method, as a lump may take 5-10 years to form before you can palpate it on your own.
Pros:
- This is obviously a DIY at-home method.
- You take charge of your own screening.
- It takes 5-10 minutes once a month.
Cons:
- Many women are confused about what they are feeling – is it a cyst, is it natural breast tissue with all the expected contouring?
- It takes 5-10 years for a lump to form.
- Lumps can change over the course of the month due to menstrual cycles.
Mammogram
Mammography is one of the most well-known and widely used breast cancer screening methods. It involves taking X-ray images of the breast tissue to detect abnormalities, such as tumors or cysts. Mammograms are recommended for women starting at the age of 40, although earlier screening may be recommended for those with a family history of breast cancer.
Pros:
- Widely available and paid for by some insurance.
- Can detect small tumors that may not be felt during a breast self-exam.
Cons:
- Mammograms detect anatomical changes, and lumps, that can take up to 5-10 years to form.
- Limited effectiveness in women with dense breast tissue. Approximately 40-50% of women have dense breast tissue, which can make mammography less effective at detecting tumors (Boyd et al., 2007).
- The FDA now admits that there are serious adverse events.
- Exposes patients to significant radiation (1000x more than a chest x-ray), which is itself cancer-causing. In fact, over 1,000 new cases of breast cancer annually are caused by mammograms.
- Does not reduce mortality – 1 in 200 women, 1 will avoid dying, 10 will be overdiagnosed.
- Leads to over-diagnoses in 48.3%.
- Can increase anxiety due to the large number of false positives. In, there’s a significant amount of misdiagnoses and missed diagnoses.
- Smashes your breast, and experts have felt this bruising can cause cancer.
- Those with the BRCA gene, who are often recommended to have more screenings, are at higher risk for cancer from this modality.
- Cannot detect changes in the armpit.
Ultrasound
Breast ultrasound uses high-frequency sound waves to create images of breast tissue. It is often used as a complementary screening tool when mammography results are inconclusive or for further evaluation of abnormalities found during a mammogram.
Pros:
- No radiation exposure.
- Effective in evaluating dense breast tissue. A study in the Journal of Clinical Oncology found that ultrasound can improve the detection of breast cancer in women with dense breasts (Berg et al., 2008).
- Can distinguish between solid masses and fluid-filled cysts.
Cons:
- Less effective as a standalone screening method.
- Highly dependent on the operator’s skill and experience.
MRI (Magnetic Resonance Imaging)
Breast MRI uses magnetic fields and radio waves to create detailed images of the breast. It is often recommended for women at high risk of breast cancer due to factors such as a strong family history or known genetic mutations.
Pros:
- High sensitivity in detecting breast cancer. According to a study in the New England Journal of Medicine, breast MRI can detect cancers that are missed by mammography.
- No radiation exposure.
- Effective for evaluating dense breast tissue and detecting small tumors.
Cons:
- Higher cost compared to mammography.
- May produce false positives, leading to unnecessary biopsies.
- Requires a dose of heavy metals for the imaging to be effective that most are not able to detox.
- It is very expensive – $2,000 to $10,000.
- Takes up to an hour for the test.
- Is NOT early detection- again, it’s looking for a lump that may have taken up to 10 years to form.
- Not recommended as a routine screening tool for average-risk women.
Thermography
Thermography, also known as thermal imaging, is a non-invasive method that captures heat patterns emitted by the body. The abnormal heat patterns may indicate the presence of early physiological changes that might be indicative of a breast cancer pattern beginning to emerge. Its use as a standalone screening method is controversial in the Western medical environment. However, this is the tool that I have been using personally for over 15 years.
Thermogram /Mamogram
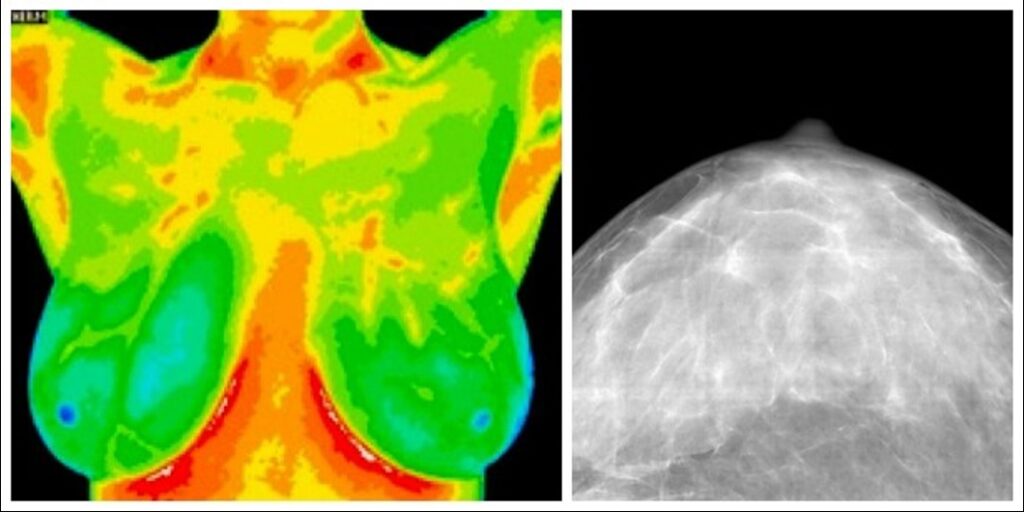
Pros:
- It’s very safe, with no radiation or compression involved.
- Non-invasive and painless.
- Whereas it detects temperature changes, it can see changes in physiology, requiring new blood vessel growth (to feed a possible tumor) 8-10 years before a lump forms.
- It is good for dense breasts and even those with implants.
- It can be used in younger women.
- Doesn’t hurt.
- It can detect early cellular changes even in the armpit area.
- It tracks changes in your breast tissue over time.
Cons:
- There is “some controversy in the literature that is as effective,” yet it was approved by the FDA in 1982 after 800 peer-reviewed studies in 250,000 women with 90% accuracy.
- Not recommended by major (western) medical organizations as a primary screening method.
QT Imaging
QT imaging is a new technology just released in 2023, that uses quantitative transmission ultrasound to create detailed images of breast tissue. It offers the promise of improved breast cancer detection without the use of ionizing radiation. This test uses a warm water bath with radio frequency to create detailed images of the breast tissue – with clarity of glands, ducts, blood vessels, and nerves.

Pros:
- No radiation exposure.
- Direct-to-consumer.
- 40x the resolution of an MRI.
- Higher sensitivity for detecting breast cancer.
- May be useful in evaluating dense breast tissue.
- You can see the biology of tissue and track changes over time, notating if diet and lifestyle change therapies are effective.
- Rare callbacks.
- FDA clearance for women that ages 18-30.
- It’s “like a spa experience,” as noted by most women who have had the test done.
Cons:
- Limited availability and research compared to traditional methods -there are now only 5 centers in the nation doing the test of the date of this publication.
- Cost and accessibility may be barriers for some individuals.
Effectiveness and Recommendations
The effectiveness of breast cancer screening methods can vary based on individual factors, including breast density, age, and risk factors, including genetics, and epigenetics (diet and lifestyle).
The PINK campaign is still advocating for Mammograms to be the “gold standard” and suggests that women start these scans starting at age 40. I did have mammograms in my early 40’s. I did have false positives, and I did have to have a biopsy. I did go through the incredible psychological stress associated with all of that. Once I discovered Thermography, over 15 years ago, I do a thermogram every 6 months to detect changes. And I’m thrilled to say that when I did see changes that were indicative that my breast health was being compromised, I was alerted early. I chose an MRI, which revealed two lumps. I chose NOT to have a biopsy just in case it was malignant disease, I did not want it spread from an encapsulated area. I chose the Oncoblot blood test, which revealed these lumps were benign. (Praise the Lord!!) I did the necessary diet and lifestyle interventions, and 6 months later, the two lumps that I had were gone. GONE! In the ensuing 10 or more years, my thermogram continues to improve!
Conclusion
Early detection is critical to improve your treatment options if, indeed, you do have malignant breast disease. Ultimately, the choice of screening method should be made in consultation with your healthcare provider, taking into account your individual risk factors and preferences.
Again, next week, I will discuss the early, functional, healthy breast health screening methods that I use personally and recommend to my clients. These methods give you the power you deserve to have!! Stay tuned.
Additionally, I am hosting a FREE Breast HEALTH Awareness Webinar on October 25th. I’ll send more information next week. Seats are limited; thus, if you want to secure yours, register at https://LoriFinlay.com/breast-health. FYI, there will be bonuses for those who attend live.